𝐏𝐔𝐋𝐒𝐄 𝐂𝐇𝐄𝐂𝐊𝐒 with CPR.......𝗪𝐇𝐀𝐓 𝐈𝐒 𝐓𝐇𝐄 𝐁𝐈𝐆 𝐃𝐄𝐀𝐋?!?!?!
In this blog I wanted to discuss pulse checks with CPR….when its recommended and when it is not and why.
During training, working with other instructors, and in general conversations with the community, I’m finding that a lot of of people are confused as to what the recommendations are for pulse checks. So, I wanted to take time to look at the recommendations and why the American Heart Association (AHA) has different recommendations based on what course is being taken.
I will primarily be discussing the recommendations from the American Heart Association (AHA) regarding pulse checks. Their recommendations are based on the course being taken: Heartsaver, BLS, ACLS, or PALS. These recommendations will be similar to the American Red Cross (ARC) courses: ALS, PALS, BLS, and First Aid/CPR/AED.
Types of Courses/Learners
We can break down the types of courses into 3 main categories
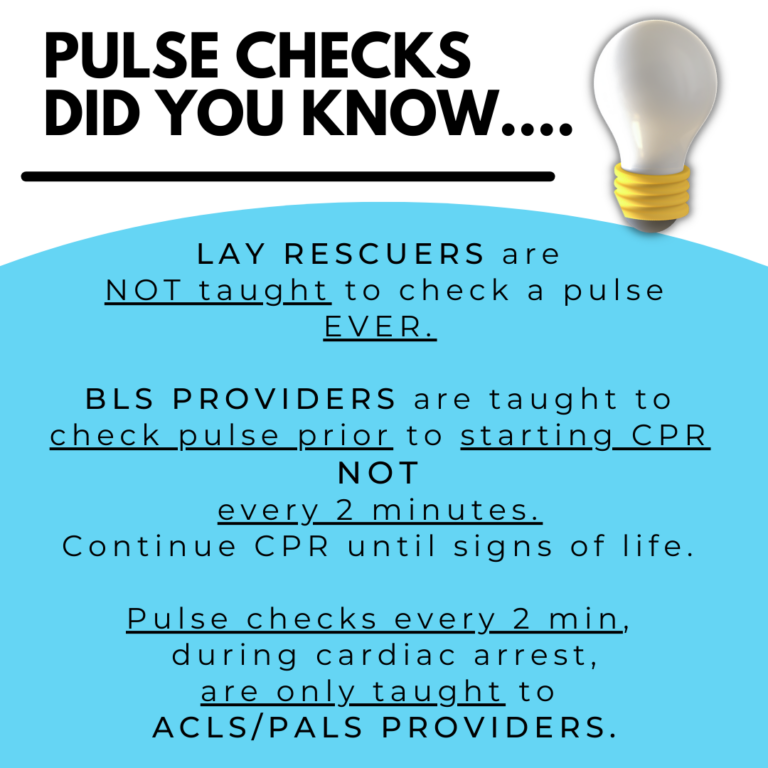
While numerous certification and non certification courses are available, they can be divided into 3 main categories for what is taught: lay rescuers, BLS providers, and ACLS/PALS providers.
Lay rescuers – are those individuals not in the healthcare setting. These recommendations will be seen in the AHA Heartsaver Certification Courses: First Aid/CPR/AED; CPR/AED; Pediatric First Aid/CPR/AED, or First Aid. You will also see these recommendations in the non-certification training: Family and Friends CPR & Hands-Only CPR.
Please note: Red Cross also has specialized training for Life Guards. Some may still refer to them as a “lay rescuers” while others may refer to them as a “professional rescuer”. Their training will be more in line with a BLS course then a “lay rescuer” CPR/AED course. They are taught a special skills set, for this higher risk environment, that is specific to the work they are doing and the lives they could be saving. Additionally, those who have had wilderness survival training will learn a different skills set. These groups should not confuse this information with the training they learned in those courses.
BLS Providers – are typically in a healthcare setting (although anyone can take this course). For example: nurses, physicians, dental hygienist, dentist, occupational therapist, speech therapist, physical therapist, EMS professionals, etc…just to name a few.
ACLS (ALS)/PALS Providers – are providers in the healthcare setting operating at the most advanced level of cardiopulmonary resuscitation. For example: nurses, physicians, physician assistants, oral surgeons, anesthesiologists, etc.
For All the wonderful Instructors out there
We should strive to know what the different recommendations are (for the courses we teach) and not confuse the learner because we may be more experienced, in our field, and do things differently.
For example, critical care providers who teach ACLS/PALS, we should not expect a lay rescuer or BLS provider to operate like we do in the critical care setting. They do not have the knowledge, training, or available resources to operate at that level. Therefore, different recommendations are presented in those courses. One is not necessarily better than another. The recommendations are based on the best that person can do with the given set of circumstances. It will always be best for a cardiac arrest to happen in critical care (ICU, CCU, ER, etc).
What are the recommendations for pulse checks with CPR?
lets look at what the recommendations are
Lay rescuers – are NOT taught to check a pulse…..EVER. You are to assume cardiac arrest if a person is unresponsive and not breathing. Call 911 and start CPR immediately.
ACLS/PALS providers – are taught are taught to check a pulse with a rhythm check every 2 minutes. We are adjusting our treatment of the patient based on the type of rhythm and presence of pulse. However, in effort to reduce long delays with these frequent checks, AHA started teaching in 2020 to identifying the pulse, with CPR, then stop to see if pulse remains or goes way.
Every 1 minute without CPR, when needed, decreases a persons survival by
7-10%
So why the different recommendations?
Goal is to increase survivability by reducing time wasters
1) Don’t spend more than 10 seconds trying discern a pulse to initiate CPR. Start compressions as quickly as possible as we know that every 1 minute that CPR is not started, when needed, a persons chance of survival decreases by 7-10%.
Yes……some pauses, during CPR, are necessary. The aim is reduce how long and how often those pauses occur. Lets be honest, discerning a pulse can be difficult, even for the experienced healthcare provider.
Identifying a pulse is difficult, even for the experienced healthcare provider
Is finding a pulse that difficult?
so now you may be asking yourself……is finding a pulse that difficult?!?!?!
The answer is yes and no.
If you take your own pulse, right now, then maybe not. But have you ever been in an emergency situation with adrenaline flowing? Your pulse is rapid and pounding. Your thought process is not as clear.
I have also witnessed countless delays in compressions surrounding difficulty discerning a pulse. This is one reason a lot of us will use a doppler (ultrasound) during cardiac arrest codes. So lets face it….identifying a pulse is difficult even for the experience healthcare provider. This is why AHA implemented several changes to BLS, ACLS, and PALS in 2020 to reduce these delays.
So, in summary:
Pulse checks can be difficult.
There are different recommendations for who does pulse checks and when.
The goal is to avoid delays or prolonging compressions for pulse checks with CPR.
THANK YOU
Hope you enjoyed the post.
Please leave a comment below and click the link to learn more about taking a course with
CPR Done Right.

